Understanding the Cancer Patient’s Treatment Journey

Cedars-Sinai Tower Hematology Oncology
The intricate interplay between the built environment and its occupants is particularly vital in the context of healthcare. To truly advance healthcare facility design, it is essential to examine how the design of the physical space directly impacts patient health outcomes. By synthesizing this effort with insight into our clients’ evolving challenges, architects can improve the treatment experience through research-informed design. This approach is especially imperative for the design of cancer treatment centers.
Advisory Board analysis indicates cancer cases are projected to increase 13% nationwide over the next decade, disproportionately affecting states with growing elderly populations. As demand for cancer care increases, health organizations face greater challenges than ever before. Staff shortages and financial instability, exacerbated during the COVID-19 pandemic, continue to strain our healthcare systems. Accordingly, new cancer facilities must be flexible, cost-effective, and innovative, with a laser focus on patient experience and high-quality care to make the most of capital investment.
With this objective in mind, I pursued a research project through SmithGroup’s Exploration Grant program. My investigation focused on the relationship between the cancer patient’s treatment journey and their preferences in infusion therapy environments, asking the core question: do space preferences change over the course of treatment?
To gain greater insight into the patient experience, I conducted a comprehensive review of the existing research and initiated a pilot program to survey patients undergoing infusion treatments in SmithGroup-designed cancer centers. The synthesis of existing research with my preliminary survey findings uncovered a nuanced perspective on infusion environments—one that has the potential to drive more informed programming strategies and more accommodative, economical, and flexible design solutions.
What the Existing Research Shows
A literature review of cancer center environments and patient experiences reveals three major themes. These themes offer a framework for analyzing variables that influence patient preferences for healing environments beyond prescribed infusion therapy.
Patient-Caregiver Relationships. The patient-caregiver relationship is crucial for trust, communication, and support. Because infusion therapy can be mentally and physically taxing, caregivers play a vital role beyond clinical duties. Staff who show genuine interest in patients’ well-being and provide empathetic support uplift the patients’ experience. Newer patients benefit and learn from conversations with caregivers and fellow patients. Both the physical proximity of caregivers to patients and the visibility of the care station during treatment contribute to patient perceptions of safety and a more positive treatment experience.
and the social and physical environment of the infusion space.
Social Environment. Social interactions among patients are shown to positively impact their well-being and experience. Some studies indicate that connecting with fellow patients can be even more influential than the physical environment. However, infusion environments need to offer a balanced experience; privacy, confidential interactions, and rest are also important factors for patients.
Physical Environment. The treatment environment can significantly affect patient stress and anxiety. Patients spend many hours in these spaces. Creating a sense of home, through natural light, operable windows, and control over the environment, can positively contribute to the treatment experience. Comfort, security, privacy, and autonomy over their physical environment all support the patient’s healing journey.
Patient Survey
I worked with a Michigan-based cancer center to develop and deploy the pilot patient survey, exploring the dynamic between the cancer patient’s treatment journey and preferences in treatment spaces. The anonymized survey was live for one month, empowering patients to provide valuable insight into the core research question, plus the patient-caregiver relationship, the social and physical environments, and other feedback related to their experience inside the facility.
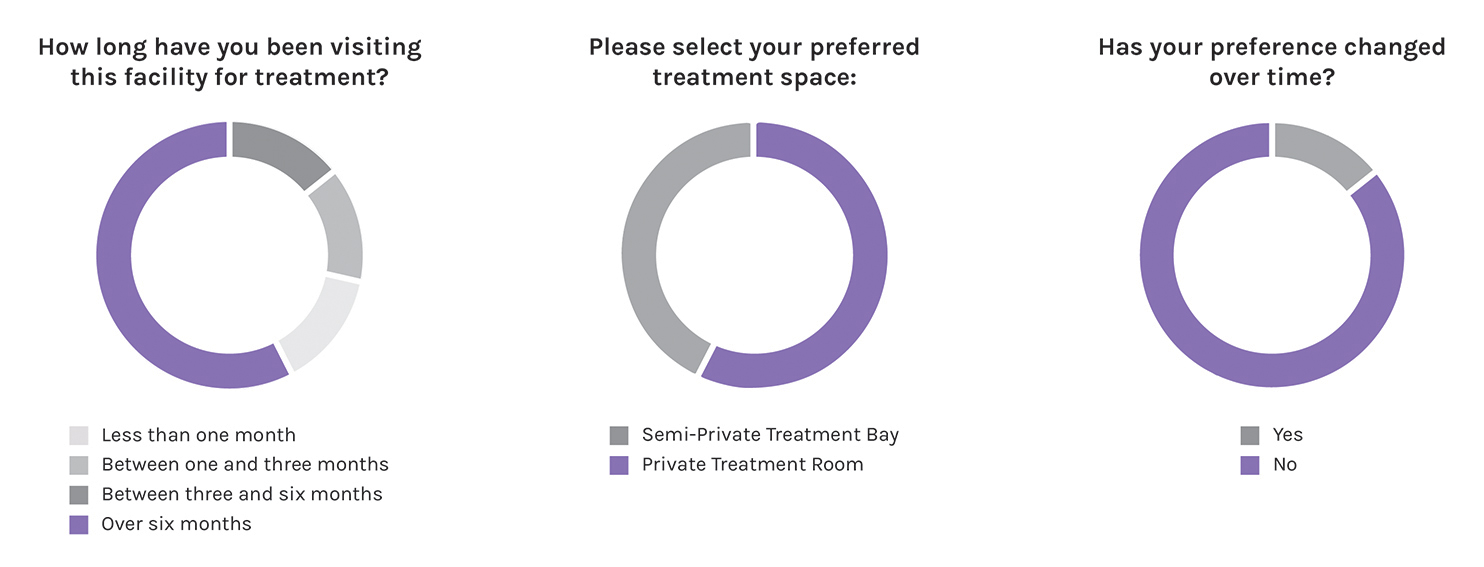
Patient Treatment Space Preferences. To test the relationship between the treatment journey and space preference, patients were asked various questions, including their personality type, how long they have been visiting the facility, their baseline preference of treatment space, and whether that preference changed over time. Responses showed that patients identifying as extroverted tend to prefer semi-private treatment spaces. Although there was a varying range of treatment tenure among the respondents, their preference of treatment space did not change over time.
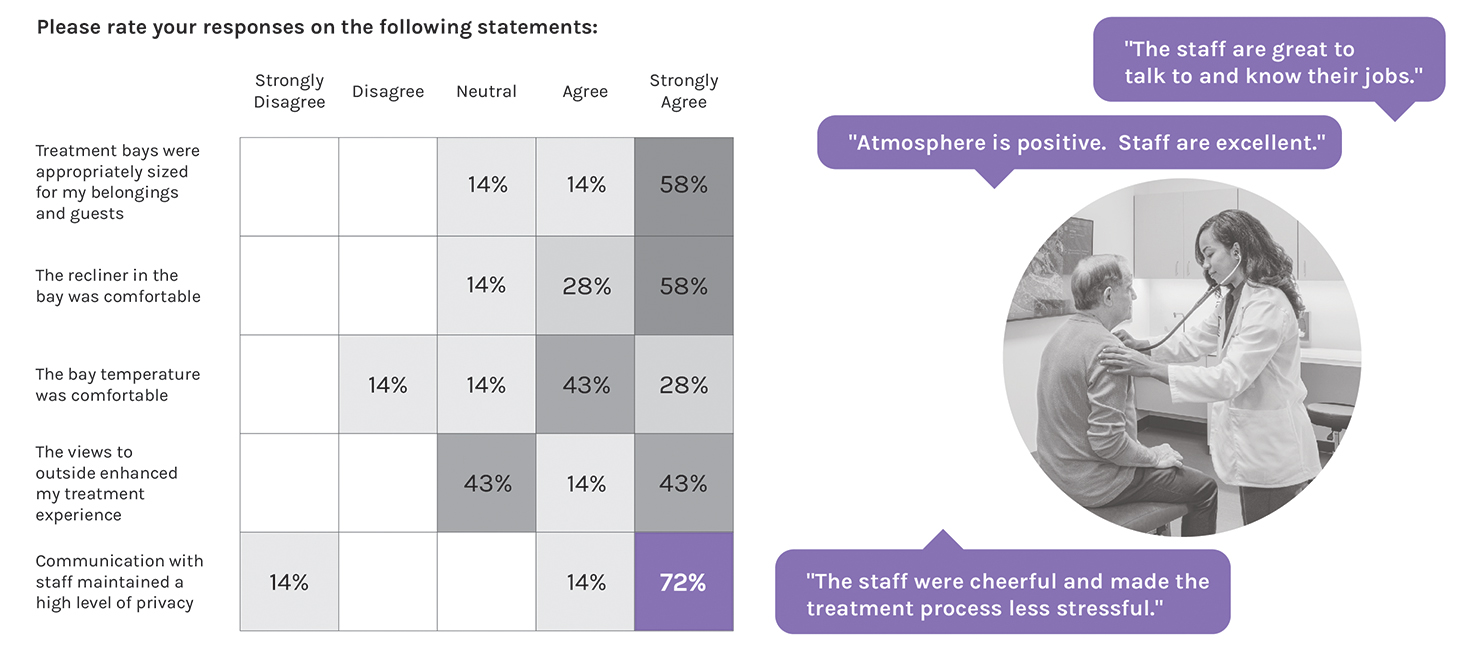
Patient Responses to Literature Review Themes. The survey asked about the patients’ experience, including communication with staff, opportunities for socialization, and the infusion room itself. Patient feedback shows that private communication with staff alleviated stress and contributed positively to their experience. Patients responded less positively to the social environment. Responses show that less than half of patients were able to make a social connection with their neighbors. Of the respondents who made a connection, only one-third found that it strongly enhanced the treatment process.
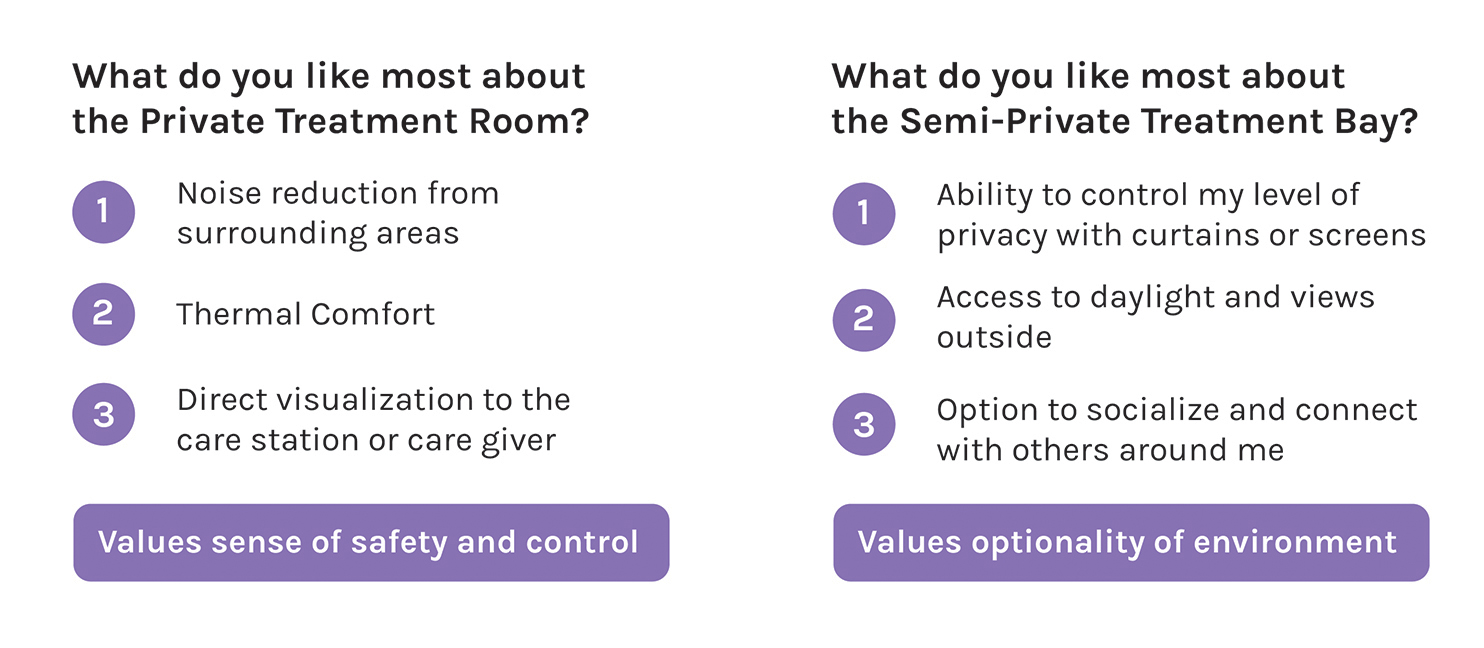
Finally, patients were asked to select what they liked most about their preferred treatment space: a private room or a semi-private treatment bay. Private room responses indicated that noise reduction, thermal comfort, and proximity to the care station are top priorities. Semi-private treatment bay responses identified privacy control, access to daylight and views, and opportunities for socialization as their top preferences.
Analysis of Survey Findings
Contrary to my initial hypothesis, patient preferences toward their therapy environment remained consistent throughout their treatment journey. This indicates that caregivers should empower patients to choose their preferred therapy space at the start of their treatment journey, and healthcare facilities should offer diverse options. Additional findings include:
- Physical adjacency and visual connection between the caregiver station and patient infusion play a vital role in providing a positive treatment experience.
- The patient-caregiver relationship has a significant impact on the patient’s overall satisfaction with the treatment process and can be supported by treatment space design.
- The patient-to-patient social dynamic was not as important as previous research indicated, potentially due to a multitude of factors, including the paradigm shift in how patients perceive their health and safety in a post-pandemic world.
- Treatment spaces that enable patient control over their own environment provide a more positive experience.
New Inquiries for Future Research
Additional focus on the patient-to-patient social dynamic is warranted due to the wide discrepancy in results from my survey compared to the existing research conducted before 2020. This discrepancy may be due to multiple factors, including:
- The design, layout, and treatment room types available for patients in the test site.
- A shift in perception of safety and comfort in a post-pandemic era as immunocompromised patients are less likely to socialize with others.
- Advancements in mobile and smart device technology that provide more options for personal engagement and entertainment during treatment.
- Cultural and regional differences.
Gathering caregiver input on their experiences and perceptions of infusion spaces would help garner insight into patient preferences and add to our understanding of how those environments can better support staff. Nationwide nursing shortages pose significant challenges to the healthcare industry; designing spaces that can reduce burnout and positively impact workplace experience and satisfaction is imperative.
While it is not possible to draw generalizable conclusions from the pilot survey without further study, initial findings point toward the benefits of identifying a patient’s preferred type of therapy space at the start of their treatment journey. As more patient data is gathered, further analysis can establish new findings and insights to inform programming and design strategies.
In the meantime, it is critical that caregivers offer patients agency over the selection of their treatment space. The healthcare facility should support a variety of spaces that balance considerations for privacy, safety, connection, control, and comfort. The most successful treatment journeys for cancer patients, and the most promising design directions for cancer centers, will all begin by posing thoughtful questions emphasizing better patient understanding and empathy.