IdeaLab: The Driverless Clinic
SmithGroup's IdeaLab is a research and innovation process that gives us the creative space—outside of everyday project concerns—to study future healthcare and other industry disruptors in depth. As part of this initiative, we explore the inventions, products, technologies, and strategies that are in the pipeline (or not yet imagined) to anticipate what these will mean for the industry and, most importantly, for our clients.
Our first IdeaLab exploration is focused on Artificial Intelligence (AI). Industry experts and three teams of SmithGroup health professionals convened to imagine what true potential lies within AI and how it could disrupt the healthcare industry—both for better and for worse—today, tomorrow and decades down the road. The IdeaLab teams were presented with this challenge: can you design a clinic, for the year 2035, that is run entirely by an artificial intelligence, with little or no human-to-human interaction?
Artificial Intelligence (AI) may seem like something out of science fiction, but its real-life counterpart is already changing how we live. We focused our exploration on ‘machine learning,’ a subset of artificial intelligence that gives computers the ability to learn new information or tasks without being explicitly programmed, using algorithms to produce deep learning neural networks that are modeled on the structure of the human brain.
SETTING THE STAGE
As the payer system shifts towards value-based care and population health, healthcare delivery systems are reorganizing themselves to provide more efficient and profitable care. The trends have been towards vertical and horizontal integration, with payers and providers blending into one in order to remain profitable in a world where incentives reward keeping patients healthy and out of the hospital. Healthcare systems are also expanding horizontally so they can provide the kind of coordinated care that will make value-based care a feasible business model.
Integrated models such as Kaiser Permanente or Group Health, where the provider is the payer, will likely become more prevalent, and the emphasis on treating episodes of care as a package rather than a separate set of symptoms treated in silos will be the norm. With population health, there will be an emphasis on keeping people well in order to make healthcare a profitable business. A growing recognition by payer/providers that the social determinants of health influence wellness and, as a consequence, healthcare expenditures, will shift the focus to addressing issues of access to preventative factors, including physical activity, healthy food, and a social support network.

Kaiser Permanente is a physician-driven organization that allows the health plan, the hospital and the physicians and medical group to work together in a coordinated fashion for the benefit of the patient.
Policy and technology are pushing healthcare in a new direction; this will have a tremendous impact on the spaces that our clients will need in just the next few years.
The Driverless Clinic
Each team was given a pre-determined persona to focus our efforts. Our persona is Peter, a 68-year-old auto assembly plant retiree who lives in the suburbs of Chicago. Peter is a widower, has children living in a different city, and a few close to a few friends locally. Even though Peter is relatively healthy and active, he has a family history of prostate cancer and high blood pressure. Peter avoids going to the doctor unless strictly necessary: the last time he did so was for a crown replacement three years ago. Peter is also frugal when it comes to spending on technology. All of this, coupled with his aversion to doctor visits, makes him a particularly challenging subject for an exercise that focuses on the role of artificial intelligence in healthcare.
Peter's care scenario starts when his biosensor identifies abnormal levels of PSA in his blood, notifies Peter and his caregiver, and gives Peter a series of options for scheduling an appointment. Our scenario assumes that Peter’s wearable has already detected an abnormality in either his urination pattern or PSA levels, and the AI has determined that further testing is needed to verify whether cancerous cells are present.
Peter's Timeline: The team mapped out a 20-year timeline, where Peter is 59 years old in 2016. This allowed us to assess technological and societal drivers that occurred during the first part of the timeline and then predict what’s expect for the latter part.
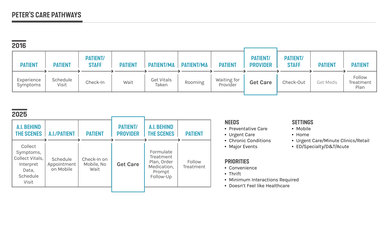
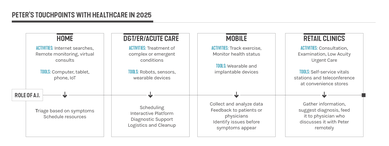
Peter's Touchpoints: Given the connected and wellness-focused environment we envision for 2025, the team determined that most of Peter’s care for minor ailments would occur in his home via a remote connection to his provider, whether by wearable or embedded devices. More pressing symptoms, such as a twisted ankle or a high fever, would be addressed at a retail clinic such as CVS. Dr. Robert Wachter, author of “The Digital Doctor,” predicts that if Peter had a problem that would today send him to an acute care unit, in the future he may be able to stay home and be monitored remotely by his care team. The only reason Peter would have to visit a physical healthcare facility in 2025 will be if he needs emergency care (such as trauma), highly specialized diagnostics that needed to be guided by technicians, highly specialized surgeries, or intensive treatment for diseases such as cancer.
In our imagined 2025, a visit to the local wellness center to get a biopsy is not much different than meeting friends at the local community center. Peter walks up to a bar, gets a drink and a small capsule with an ingestible diagnostic sensor in it, and can enjoy a range of activities at the center while the biopsy is taking place. All the medical aspects of the visit are invisible to Peter. Information is wirelessly transferred from his smartphone and wearable to the AI, and doctors and physicians monitor the AI feed behind the scenes.

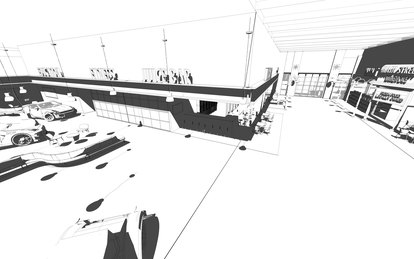
The team imagined a wellness center consisting of three zones: Lifestyle, Wellness, and Provider/Staff Support. The Lifestyle zone is a high activity area that incorporates entertainment and retail amenities to encourage camaraderie. We integrated the principles of Danish ‘Hygge’ design—“the absence of anything annoying or emotionally overwhelming; taking pleasure from the presence of gentle, soothing things”—into what we are referring to as the Wellness zone, a lower activity area. Lastly, the Provider/Staff area is practically invisible to the rest of the center, although there is a physical connection to the Wellness zone for functions that overlap.

Our clinic concept could be integrated into a future urban environment, perhaps by redeveloping a traditional suburban shopping center, taking into account future requirements for autonomous vehicles. This concept creates a walkable environment, encouraging activity not only inside the building but throughout the entire site.
Conclusion
After researching technological, policy, industry and societal trends, our team found that the common thread among the key findings is that less space will be needed for examination, procedures and administrative tasks, and more space will be focused on human interactions and wellness activities. They also recognized that to capture patients and motivate them to stay well, the nature of health facilities needs to change from places where people have to go to places where people want to go. Although our artificial intelligence clinic is 'driverless,' with much more automated medical functions disappearing into the background, we believe the future of medical care is still very much a humanistic endeavor.
Learn more about IdeaLab or the IdeaLab teams' findings, A Smart Clinic Empowered by Data, and Better Access through AI. Download our full report here.